Is Cervical Cancer Genetic?
Is Cervical Cancer Genetic?

Cervical cancer is one of the most common cancers affecting women worldwide, but its causes are often misunderstood. A common question many people ask is whether cervical cancer is genetic. While cervical cancer does not typically run in families the way some other cancers do, there are genetic and environmental factors that play a role in its development. This blog explores the complex relationship between genetics, lifestyle, and other risk factors associated with cervical cancer.
What Is Cervical Cancer?
Cervical cancer arises in the cells of the cervix, which is the lower part of the uterus connecting to the vagina. The primary cause of cervical cancer is persistent infection with high-risk types of the human papillomavirus (HPV), a common sexually transmitted virus. Although most HPV infections clear up on their own, certain strains can cause cellular changes in the cervix, eventually leading to cancer.
Cervical cancer is generally classified into two main types:
- Squamous cell carcinoma: This accounts for the majority (about 90%) of cervical cancer cases.
- Adenocarcinoma: This arises in the glandular cells of the cervix and is less common but potentially more aggressive.
The Role of Genetics in Cervical Cancer
1. Inherited Genetic Factors
Unlike hereditary cancers such as breast or ovarian cancer linked to BRCA gene mutations, cervical cancer is rarely considered a hereditary condition. However, genetic susceptibility can play a minor role. For instance:
- HLA (Human Leukocyte Antigen) genes: These genes are involved in the immune system’s ability to recognize and clear HPV infections. Variations in certain HLA genes may make some individuals less effective at clearing HPV, increasing their risk of persistent infection and subsequent cancer development.
- Other genetic polymorphisms: Research has identified several genetic variations in genes associated with DNA repair, immune response, and cell cycle regulation that may influence a person’s risk of developing cervical cancer.
These cervical cancer genetic predispositions, however, typically interact with environmental and lifestyle factors, such as HPV exposure, smoking, and immune system health.
2. Somatic Genetic Mutations
While inherited genetic factors play a minor role, genetic changes (mutations) in cervical cells acquired over a person’s lifetime are critical in the development of cervical cancer. These changes are often triggered by HPV infection but can also result from other factors such as smoking or chronic inflammation. Common genetic alterations in cervical cancer genetics include mutations in:
- TP53: This tumor suppressor gene helps regulate cell growth and prevent cancer. HPV can inactivate TP53, allowing abnormal cells to grow uncontrollably.
- PIK3CA: Mutations in this gene can drive cancer progression by promoting abnormal cell growth and survival.
HPV: The Main Culprit Behind Cervical Cancer
The overwhelming majority of cervical cancer cases are linked to high-risk HPV types, particularly HPV-16 and HPV-18. HPV infection is not genetic but acquired through sexual contact. Certain factors can increase the risk of acquiring or failing to clear an HPV infection, including:
- Early age at first sexual intercourse
- Multiple sexual partners
- Weakened immune system (due to conditions like HIV or immunosuppressive therapy)
- Long-term use of oral contraceptives
While HPV is the primary driver, not all women with HPV develop cervical cancer. This is where other risk factors, including genetic susceptibility, come into play.
Environmental and Lifestyle Factors in Cervical Cancer Risk
1. Smoking
Smoking doubles the risk of cervical cancer. Tobacco by-products can damage the DNA in cervical cells and weaken the immune system’s ability to fight HPV infections.
2. Weakened Immune System
A compromised immune system, due to HIV infection or certain medications, reduces the body’s ability to clear HPV infections, increasing the risk of cervical cancer.
3. Diet and Nutrition
A diet low in fruits and vegetables may affect overall immune function, potentially increasing susceptibility to persistent HPV infections and cervical cancer.
4. Long-Term Contraceptive Use
Studies suggest that long-term use of oral contraceptives may slightly increase cervical cancer risk, though the exact mechanism is not fully understood.
Prevention: Reducing the Risk of Cervical Cancer
1. HPV Vaccination
Vaccines such as Gardasil and Cervarix protect against the most common high-risk HPV types (16 and 18) and significantly reduce the risk of cervical cancer. The vaccine is most effective when administered before exposure to HPV, typically in preteens.
2. Regular Screening
Routine Pap smears and HPV tests can detect precancerous changes in cervical cells, allowing for early intervention. Women should follow screening guidelines based on their age and medical history.
3. Safe Sexual Practices
Using condoms and limiting the number of sexual partners can reduce the risk of HPV transmission.
4. Quitting Smoking
Smoking cessation improves overall health and reduces cervical cancer risk.
5. Healthy Lifestyle
Maintaining a balanced diet, exercising regularly, and boosting immunity through a healthy lifestyle can help the body clear HPV infections more effectively.
What to Do If You Have a Family History of Cervical Cancer
While cervical cancer is not considered hereditary, a family history of the disease may indicate shared lifestyle or environmental factors, or a genetic predisposition to immune or DNA repair inefficiencies. If you have a family history of cervical cancer:
- Inform your healthcare provider.
- Follow recommended screening protocols rigorously.
- Consider genetic counseling if you suspect an underlying hereditary syndrome (though rare for cervical cancer).
Conclusion
So, is cervical cancer genetic? The answer is complex. While genetic predispositions can influence susceptibility to HPV infection and progression to cancer, cervical cancer is not typically hereditary in the way some other cancers are. The primary cause of cervical cancer is persistent infection with high-risk HPV types, influenced by environmental and lifestyle factors.
The good news is that cervical cancer is largely preventable through HPV vaccination, regular screening, and lifestyle modifications. By understanding the interplay between genetics and external factors, women can take proactive steps to protect themselves from this disease.
Remember, knowledge is power. Spread awareness about the importance of HPV vaccination and regular cervical cancer screenings to help reduce the global burden of this disease.
Foods to Boost Fertility
Discover foods to boost fertility, learn how nutrition impacts reproductive health & get tips for a…
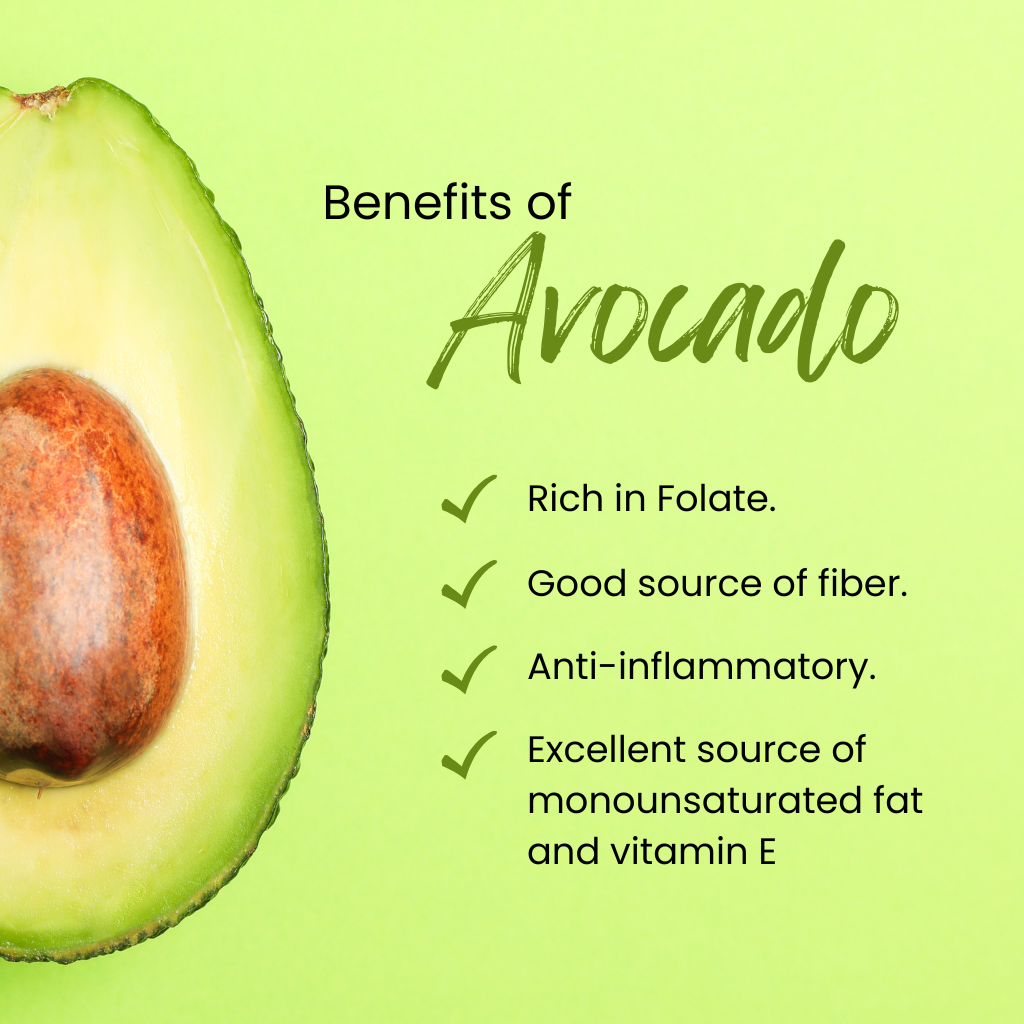
Avocado benefits
discover the incredible Avocado Benefits! from heart health and glowing skin to improved digestion and brain…
Is Cervical Cancer Genetic?
Cervical cancer isn't usually hereditary, but genetic susceptibility, HPV infection, and lifestyle factors influence risk. Prevention…